St. John’s Wort drug interactions are among the most significant in herbal medicine because the supplement acts as a potent inducer of the CYP3A4 liver enzyme and the P-glycoprotein transporter. This metabolic acceleration causes the body to process and eliminate medications too quickly, drastically reducing the efficacy of critical drugs such as birth control pills, blood thinners like warfarin, immunosuppressants, and antiretrovirals, while simultaneously posing a risk of serotonin syndrome when combined with SSRIs.
The Mechanism: How St. John’s Wort Alters Metabolism
To understand the severity of St. John’s Wort (Hypericum perforatum) interactions, one must understand the pharmacokinetics behind its active constituents. Unlike simple dietary supplements that may have mild additive effects, St. John’s Wort fundamentally changes how the human liver processes xenobiotics (foreign chemical substances). The primary driver of this activity is hyperforin, a phytochemical unique to this plant.
Hyperforin and Serotonin Reuptake Inhibition
Hyperforin is believed to be the primary antidepressant component of St. John’s Wort. Its mechanism of action mimics that of synthetic antidepressants, specifically Selective Serotonin Reuptake Inhibitors (SSRIs). Hyperforin inhibits the reuptake of serotonin, dopamine, and norepinephrine in the neuronal synapse, increasing the availability of these neurotransmitters to improve mood.
While this mechanism is beneficial for treating depression, it creates a direct pharmacodynamic conflict when a patient is already taking prescription antidepressants. Since both the herb and the drug are attempting to increase serotonin levels, the cumulative effect can lead to toxicity, a condition known as serotonin syndrome. This is not merely a side effect but a medical emergency characterized by neuromuscular hyperactivity, autonomic instability, and altered mental status.
The CYP3A4 Induction Pathway
The most profound impact of St. John’s Wort lies in its effect on the cytochrome P450 enzyme system, specifically the CYP3A4 isoenzyme. This specific enzyme is responsible for metabolizing approximately 50% of all marketed medications. St. John’s Wort acts as a potent inducer of CYP3A4.
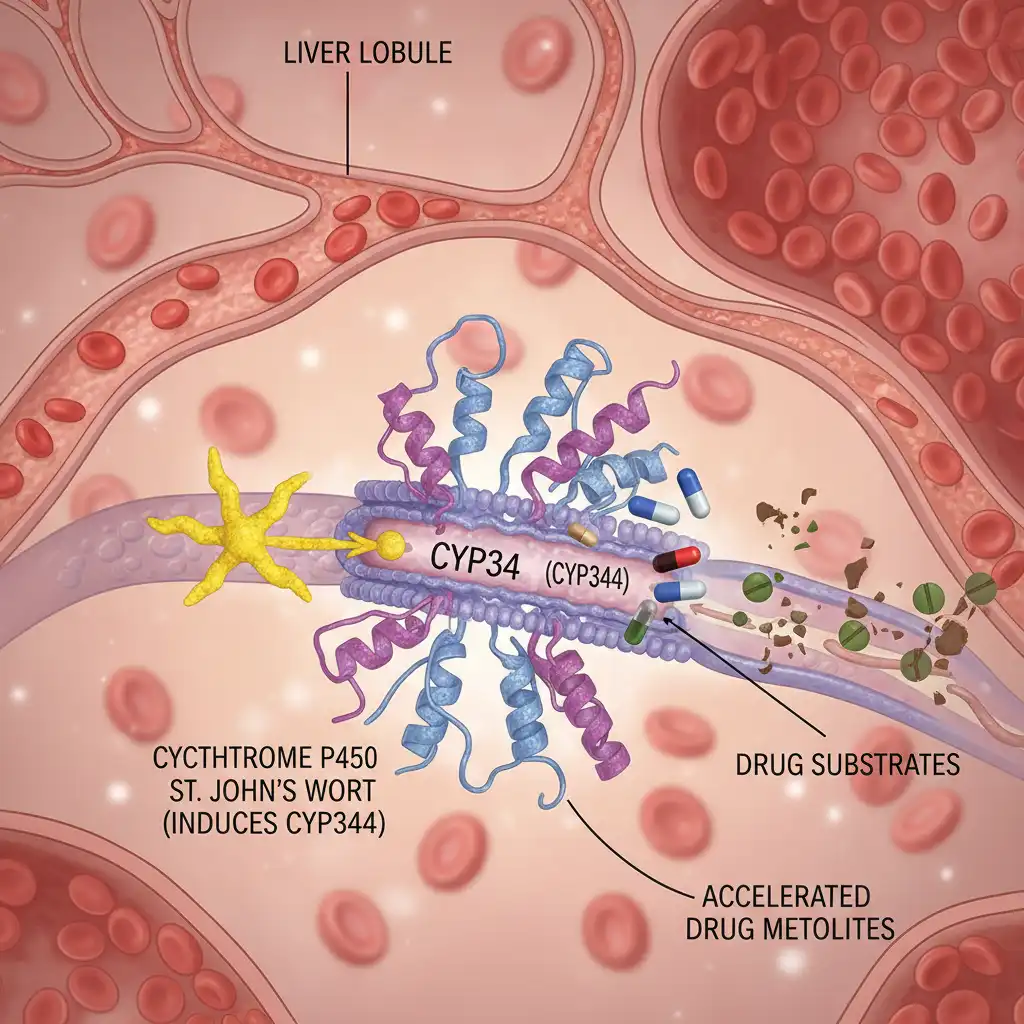
When a substance induces an enzyme, it stimulates the liver to produce more of that enzyme. Consequently, any other drug metabolized by that pathway is broken down and eliminated from the body much faster than intended. This leads to sub-therapeutic levels of the medication, rendering it ineffective. Furthermore, St. John’s Wort induces P-glycoprotein (P-gp), a transport protein that pumps drugs out of cells, further reducing drug absorption in the gut. This dual-action mechanism—enhanced metabolism and reduced absorption—is why St. John’s Wort is contraindicated with such a vast array of pharmaceuticals.
Critical Drug Interactions and Safety Risks
The scope of interactions involving St. John’s Wort is extensive. In integrative health, practitioners must be vigilant, as patients often do not report herbal supplement use to their primary care physicians; referencing Best Practices for Selling Herbal Products Online in NZ is essential for industry compliance. The following categories represent the highest risk profiles.
Hormonal Contraceptives and Birth Control
One of the most documented and consequential interactions is with oral contraceptives. Because St. John’s Wort accelerates the metabolism of ethinyl estradiol and progestins via CYP3A4 induction, it can lower hormone levels in the blood below the threshold required to prevent ovulation. This can result in breakthrough bleeding and, more critically, unintended pregnancy. Women relying on hormonal birth control (including pills, patches, and rings) should generally avoid St. John’s Wort to ensure contraceptive reliability.
Blood Thinners (Anticoagulants)
For patients managing cardiovascular conditions, the interaction with warfarin (Coumadin) is dangerous. Warfarin has a narrow therapeutic index, meaning small changes in blood levels can lead to clots (if levels are too low) or hemorrhage (if levels are too high). St. John’s Wort increases the elimination of warfarin, causing a decrease in the International Normalized Ratio (INR). This leaves the patient vulnerable to thrombotic events, such as stroke or pulmonary embolism. According to the National Center for Complementary and Integrative Health (NCCIH), combining these therapies requires strict medical supervision, though total avoidance is usually recommended.
SSRIs and MAOIs
As previously mentioned, combining St. John’s Wort with prescription antidepressants creates a risk of serotonin syndrome. This applies to:
- SSRIs: Fluoxetine (Prozac), Sertraline (Zoloft), Paroxetine (Paxil).
- Tricyclic Antidepressants: Amitriptyline, Nortriptyline.
- MAOIs: Phenelzine, Tranylcypromine.
Symptoms of serotonin syndrome range from mild shivering and diarrhea to severe muscle rigidity, fever, and seizures. A “washout period” is typically required when switching between St. John’s Wort and prescription antidepressants.
Immunosuppressants and Transplant Rejection
Perhaps the most life-threatening interaction involves immunosuppressive drugs like cyclosporine and tacrolimus, used by organ transplant recipients. St. John’s Wort can drastically reduce blood levels of these drugs, leading to acute organ rejection. There have been documented cases where patients lost transplanted hearts or kidneys solely due to the addition of St. John’s Wort to their regimen.
Clinical Efficacy: Mild vs. Major Depression
Despite the interaction profile, as noted on our Home page, St. John’s Wort remains a popular therapeutic option because, for the right patient, it works. The efficacy profile varies significantly depending on the severity of the depressive disorder.
Efficacy in Mild to Moderate Depression
Numerous systematic reviews, including those by the Cochrane Collaboration, have found that St. John’s Wort extracts are superior to placebo and similarly effective to standard antidepressants for the treatment of mild to moderate depression. In these studies, patients taking St. John’s Wort often reported fewer side effects (such as sexual dysfunction or weight gain) compared to those on SSRIs.

For patients with mild symptoms who are not taking other medications, this herbal remedy offers a viable, plant-based alternative. Other botanicals with significant clinical interest include Kawakawa: Scientific Studies & Therapeutic Potential. The therapeutic effect typically takes 4 to 6 weeks to manifest, similar to pharmaceutical options.
Limitations in Major Depressive Disorder (MDD)
The data is far less compelling for severe major depression. In cases where depression involves suicidal ideation, psychosis, or severe functional impairment, St. John’s Wort is generally considered insufficient. The variability in potency between different product batches makes it unreliable for high-stakes psychiatric management. Furthermore, the risk of delaying effective pharmaceutical treatment can be detrimental to patients with severe MDD.
Dosage, Standardization, and Regulation
One of the challenges in natural medicine is the lack of strict regulation compared to pharmaceuticals. In the United States, the FDA regulates St. John’s Wort as a dietary supplement, not a drug. This means manufacturers do not need to prove efficacy before marketing.
To mitigate this, consumers and practitioners should look for standardized extracts. The most studied formulations are standardized to contain:
- 0.3% Hypericin: While hypericin was originally thought to be the active ingredient, it is now used primarily as a marker for standardization.
- 2-5% Hyperforin: As the primary active constituent for antidepressant effects and drug interactions, hyperforin content is crucial.
Typical dosages in clinical trials range from 300 mg to 900 mg daily, usually divided into three doses. However, “high-potency” formulations may carry higher risks of interaction.
Guidelines for Safe Integrative Use
Integrative health professionals must adopt a safety-first approach when recommending St. John’s Wort. The potential for harm does not negate the herb’s value, but it necessitates strict protocols.
- Comprehensive Medication Review: Before starting St. John’s Wort, a complete audit of the patient’s current medications, including over-the-counter drugs and other supplements, is mandatory.
- The “Washout” Rule: If a patient is transitioning from an SSRI to St. John’s Wort, a physician-supervised taper and washout period is necessary to prevent serotonin syndrome.
- Pre-Surgical Cessation: Due to interactions with anesthetics and blood clotting, patients should discontinue St. John’s Wort at least 5 to 7 days prior to any scheduled surgery.
- Sun Sensitivity Awareness: High doses of St. John’s Wort can cause photosensitivity (phototoxicity). Patients should be advised to use sunscreen and avoid excessive UV exposure.
For detailed safety alerts, practitioners can consult resources provided by the U.S. Food and Drug Administration (FDA) regarding dietary supplement advisories.
People Also Ask
What drugs should not be taken with St. John’s Wort?
You should avoid taking St. John’s Wort with antidepressants (SSRIs, MAOIs), birth control pills, blood thinners (warfarin), cyclosporine (anti-rejection drug), digoxin (heart medication), HIV medications (indinavir), and certain cancer chemotherapy drugs (irinotecan). The herb reduces the effectiveness of these life-saving medications.
Does St. John’s Wort cancel out birth control?
Yes, St. John’s Wort can significantly reduce the effectiveness of hormonal birth control pills, patches, and rings. It speeds up the liver’s processing of hormones, which can lead to breakthrough bleeding and unintended pregnancy. Women using these forms of contraception should use a backup barrier method or avoid the supplement.
How long does St. John’s Wort stay in your system?
The elimination half-life of hyperforin, the active component, is approximately 9 to 24 hours. However, the induction of liver enzymes (CYP3A4) caused by St. John’s Wort can persist for up to two weeks after you stop taking the supplement. Therefore, interaction risks remain for several days after discontinuation.
Is St. John’s Wort safe for high blood pressure?
St. John’s Wort is generally not a direct cause of high blood pressure, but it can interact with medications used to treat hypertension, such as calcium channel blockers (e.g., nifedipine). By reducing the effectiveness of these drugs, it could indirectly cause blood pressure to rise uncontrolled.
Can you take St. John’s Wort with ibuprofen?
Generally, there is no severe direct interaction between St. John’s Wort and NSAIDs like ibuprofen. However, since both substances can affect blood clotting mechanisms (albeit through different pathways), combining them might slightly increase the risk of bleeding in susceptible individuals. Consult a doctor if you have a history of ulcers.
What are the signs of serotonin syndrome from St. John’s Wort?
Signs of serotonin syndrome include agitation, confusion, rapid heart rate, high blood pressure, dilated pupils, loss of muscle coordination, muscle rigidity, and heavy sweating. This can occur if St. John’s Wort is taken alongside other serotonergic drugs like SSRIs or triptans.