Natural eczema remedies encompass a comprehensive, holistic approach to managing atopic dermatitis by focusing on repairing the skin barrier, rebalancing the local microbiome, and reducing systemic inflammation through dietary changes. Unlike conventional treatments that primarily suppress symptoms using corticosteroids, natural protocols aim to identify and eliminate root causes—such as gut dysbiosis, food sensitivities like gluten and dairy, and environmental toxins—to promote long-term skin health and resilience, as detailed on our Home page.
The Skin Microbiome Connection
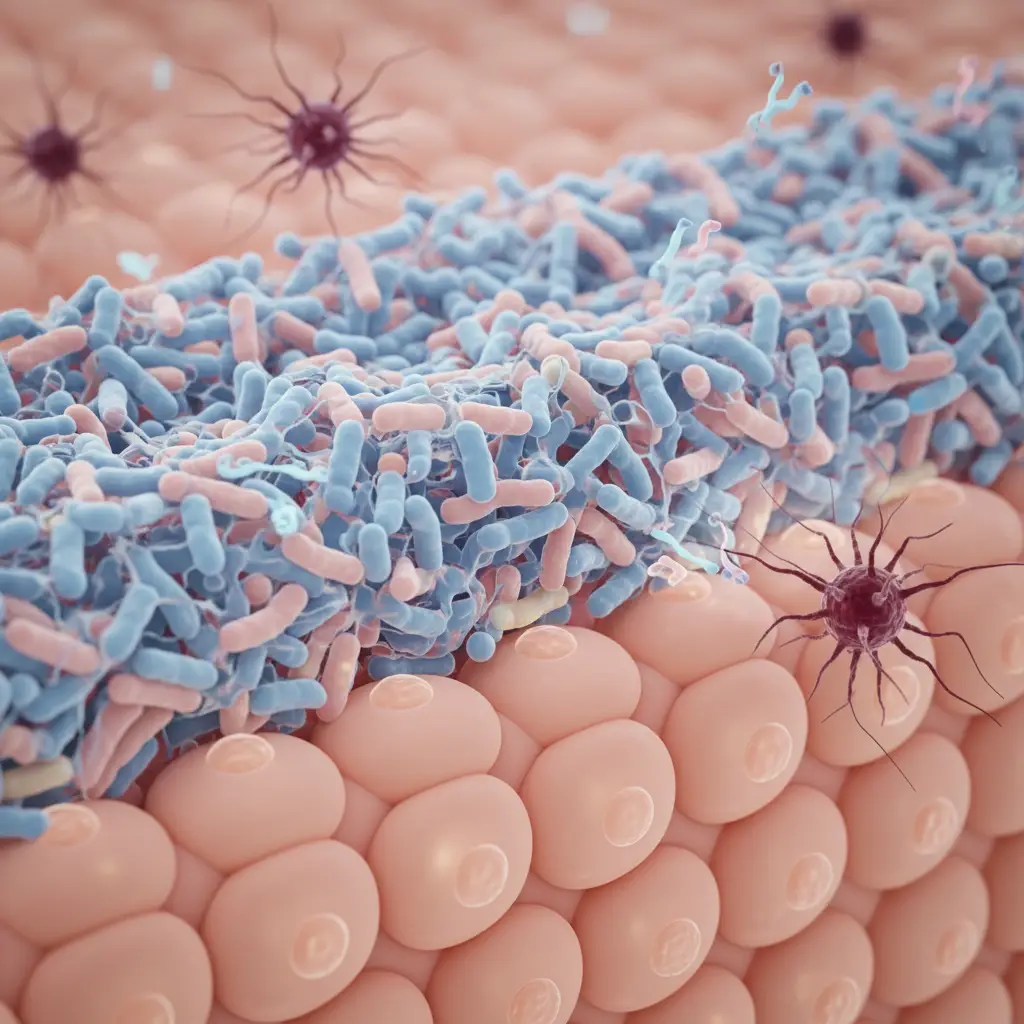
For decades, the standard of care for eczema (atopic dermatitis) focused almost exclusively on suppressing the immune system and reducing inflammation. However, modern integrative medicine has shifted the focus toward a crucial, often overlooked ecosystem: the skin microbiome. Just as the gut has a complex community of bacteria, the skin hosts trillions of microorganisms that serve as the first line of defense against pathogens.
In healthy skin, a diverse array of commensal bacteria helps maintain the acidic pH of the skin barrier (the acid mantle) and produces antimicrobial peptides. In eczema-prone skin, this diversity is often compromised. Research indicates that a significant percentage of eczema flares are associated with an overgrowth of a specific bacterium called Staphylococcus aureus. When this bacterium proliferates, it forms a biofilm that occludes sweat ducts and triggers an immune response, leading to the characteristic itch-scratch cycle.
Restoring the microbiome is a cornerstone of natural eczema remedies. This involves avoiding harsh, alkaline soaps that strip the acid mantle and instead using pH-balanced, prebiotic-friendly cleansers. By fostering a healthy microbial environment, we allow beneficial bacteria like Staphylococcus epidermidis to thrive, which naturally keeps pathogenic overgrowth in check.
Top Natural Topical Treatments for Barrier Repair
The primary physical defect in eczema is a compromised skin barrier, often linked to a mutation in the filaggrin gene, which is responsible for bundling keratin filaments. When the barrier is weak, moisture escapes (Transepidermal Water Loss, or TEWL), and allergens enter. Natural topical treatments aim to seal the barrier and replenish lipids without synthetic irritants.
Colloidal Oatmeal
Colloidal oatmeal is one of the few natural ingredients recognized by the FDA as a skin protectant. It is made by grinding oat grain into a fine powder that disperses in water. The magic lies in its chemical composition: it contains avenanthramides, which are potent anti-inflammatory compounds, and beta-glucans, which form a protective film over the skin to lock in moisture. Regular soaking in colloidal oatmeal baths can significantly reduce the histamine response and soothe irritated skin.
Shea Butter and Lipid Replenishment
To repair the barrier, one must replace the missing lipids. Shea butter, derived from the nut of the African karité tree, is exceptional for this purpose. It is rich in stearic and oleic acids, which closely mimic the natural oils (sebum) produced by human skin. Unlike water-based lotions that evaporate quickly, raw shea butter acts as an occlusive, physically blocking water loss and providing a long-lasting shield against environmental irritants.
Manuka Honey
For eczema patches that are prone to infection or weeping, Manuka honey is a powerful tool in the integrative arsenal. Sourced from New Zealand, this honey possesses unique antibacterial properties due to its methylglyoxal (MGO) content. It can help break down the biofilms created by Staphylococcus aureus while keeping the wound moist to prevent cracking and scarring.
Dietary Triggers and Anti-Inflammatory Nutrition
The saying “you are what you eat” is particularly relevant to inflammatory skin conditions. In integrative health, the skin is often viewed as a map of the gut. If the gut lining is compromised (a condition often referred to as “leaky gut” or increased intestinal permeability), large food proteins can enter the bloodstream, triggering systemic inflammation that manifests as eczema flares.

The Dairy and Gluten Connection
Two of the most common triggers for eczema sufferers are dairy and gluten. Dairy products, particularly cow’s milk, contain casein and whey proteins that can be highly immunogenic. Many individuals with eczema find that eliminating dairy leads to a significant reduction in redness and itching. Similarly, gluten—a protein found in wheat, barley, and rye—can increase zonulin production, a molecule that modulates the permeability of tight junctions in the gut. For those with non-celiac gluten sensitivity, removing gluten can be a pivotal step in healing the skin from the inside out.
The Importance of Omega-3s
To combat inflammation, the diet must be rich in Omega-3 fatty acids. These essential fats inhibit the production of inflammatory cytokines. Sources include wild-caught salmon, mackerel, sardines, flaxseeds, and walnuts. Incorporating these foods helps change the fatty acid composition of the cell membranes, making the skin more supple and less prone to dryness.
For more detailed information on the gut-skin connection, you can refer to resources provided by the National Institutes of Health (NIH) regarding the gut microbiome and atopic dermatitis.
Supplements: The Role of GLA and Vitamin D
While a whole-foods diet is the foundation, targeted supplementation can address specific metabolic blocks common in eczema patients.
Gamma-Linolenic Acid (GLA)
One of the most specific supplements for eczema is Gamma-Linolenic Acid (GLA). The body typically converts dietary linoleic acid (from vegetable oils) into GLA, which is then converted into anti-inflammatory prostaglandins (PGE1). However, many people with eczema lack the enzyme (delta-6-desaturase) required for this conversion. Supplementing directly with oils rich in GLA bypasses this metabolic block. Evening Primrose Oil and Borage Oil are the most potent sources. Clinical observations suggest that consistent use of GLA supplements can improve skin elasticity and moisture retention over 8 to 12 weeks, though users should consult the Safe Blending of Herbal Traditions: Avoiding Contraindications & Interactions before starting new regimens.
Vitamin D Optimization
Vitamin D is technically a pro-hormone that plays a vital role in immune regulation. It stimulates the production of cathelicidins, antimicrobial proteins that the skin uses to fight off infection. Deficiency in key immune regulators often requires specific support such as Oscillococcinum: Flu Symptom Management during the winter months. in Vitamin D is widespread among eczema sufferers, particularly in winter months or higher latitudes. Correcting this deficiency through supplementation (often Vitamin D3 with K2) can help modulate the immune system’s overreaction to allergens.
Lifestyle Factors: Stress and Environment
Even with the perfect diet and topicals, high stress levels can perpetuate the eczema cycle. This is known as the “neuro-immuno-cutaneous” system. Stress triggers the release of cortisol and histamine, which increases inflammation and the sensation of itching. This is why stress management techniques, such as mindfulness meditation, yoga, or deep breathing exercises, are considered essential natural eczema remedies.
Furthermore, environmental toxins play a massive role. Conventional laundry detergents often contain enzymes, optical brighteners, and synthetic fragrances that remain on fabrics and irritate the skin 24/7. Switching to non-toxic, fragrance-free, and hypoallergenic laundry options is a simple but critical change. Additionally, wearing breathable natural fibers like cotton, bamboo, or silk—while avoiding wool and synthetic polyester—can prevent mechanical irritation and overheating.

People Also Ask
What is the fastest way to cure eczema naturally?
There is no overnight “cure” for eczema, as it is a chronic condition. However, the fastest way to find relief naturally is to immediately repair the skin barrier using colloidal oatmeal baths and thick occlusive moisturizers (like shea butter), while simultaneously identifying and removing acute triggers such as harsh soaps, fragrances, or specific food allergens like dairy.
Does drinking water help eczema?
Yes, hydration is essential. While drinking water alone won’t cure eczema, systemic dehydration makes the skin more prone to dryness and cracking. Staying hydrated supports the body’s detoxification pathways and helps maintain the moisture content of the dermis, though it must be paired with topical moisturizers to lock that water in.
Which oil is best for eczema?
Coconut oil (specifically virgin, cold-pressed) and Jojoba oil are among the best. Coconut oil contains lauric acid, which has antibacterial properties against Staphylococcus aureus. Jojoba oil is technically a liquid wax ester that closely mimics human sebum, making it easily absorbed and non-irritating for sensitive skin.
Can apple cider vinegar help eczema?
Yes, diluted apple cider vinegar (ACV) can help. Eczema skin often has a higher (more alkaline) pH, which disrupts the barrier. An ACV rinse (diluted 1:10 with water) can help restore the skin’s natural acidity, improving barrier function and inhibiting bacterial growth. Never apply it undiluted, as it can burn.
What foods trigger eczema flare-ups?
The most common dietary triggers include cow’s milk, eggs, gluten (wheat), soy, and peanuts. Additionally, foods high in sugar and processed carbohydrates can spike insulin and inflammation, worsening flares. Keeping a food diary is the best way to identify individual triggers.
Is the sun good for eczema?
Moderate sun exposure can be beneficial for many eczema sufferers because UV rays stimulate Vitamin D production and have an immunosuppressive effect that reduces inflammation. However, sweat triggered by heat can be an irritant, and sunburn must be avoided, so controlled, short-duration exposure is best.

